These are my notes from a recently webinar by Dr. Andrew Ahn, an Assistant Professor of Radiology at Harvard Medical School whose research interest is in computational medicine and in large-scale electrophysiological process within the human body. He is an unpaid scientific advisor to PhysioQ, which makes measurement tech for research.
Dr. Ahn’s lecture was wonderfully clear, and I found myself taking detailed Roam notes. I’m sharing these notes below. They were taken while watching the video, with just a few later corrections, so please forgive any errors or mistakes. I have an intuition that they will be of interest to at least a few people here! This is part one of a lecture series by Dr. Ahn. Part two is being given September 13th and I’ll try to watch. If you want to watch it yourself, here are the details:
Notes from Heart Rate Variability: Antiquated or Indispensable? Part 1
- Author::Andrew Ahn
- Publication Date:: August 2021
- URL or Bibtex:: https://www.physioq.org/lesson/hrv-antiquated-or-indispensable-part-1
- [[Reference Notes]]
-
HRV is considered antiquated by clinicians, and useful by athletes and others involved in self-tracing. Interestingly, many clinicians do not know how highly valued HRV is outside the clinical setting, and many non-clinicians using HRV do not know how skeptical clinicians are of it’s utility.
-
The Zio continuous HR monitor, which is commonly used in clinical practice, does not even report HRV.
-
The last time any major guidelines or consensus paper was published was 1996. European Society of Cardiology and the North American Society of Pacing and Electrophysiology, published in European Heart Journal and Circulation. They only identified two uses: post heart attack assessment, and diagnosis of diabetic neuropathy. The only follow up was in 2015, a position paper by the some of the same group. They looked at non-linear method and found no reason to recommend them over traditional methods. It was published in a much smaller journal and wasn’t very much cited.
-
Wearable companies use HRV as a cornerstone of app functionality. Whoop Recovery measure uses HRV as one of the core measures.
-
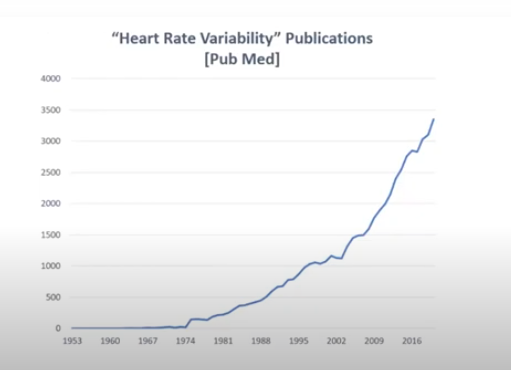
It has also become more interesting to academic researchers, even when rise of # of journals is taken into account.
- Obstetrics was the most prominent discipline in the 1980s, because of their interest in fetal heart rate monitoring.
- Then cardiology dominated 1990s and 2000s.
- Then neuroscience started to take over. Autonomic issues were the first, and then the development of neuroimaging, engineering, and sports medicine.
-
Stages: Understanding HRV, HRV as a marker of autonomic nervous system, HRV as a marker of body wide function, HRV within a construct of mind-body interaction, HRV as itself a desirable target.
-
A very good physiological description of the nervous system influence on heartbeat. I learned that the “natural” heart rate (that is a heart rate that isn’t connected to the nervous system) is rather high. They know this from humans and animals who have had heart transplants. I also liked looking at the basic schematic of influences on HRV, including central neural control and peripheral mechanical factors.
-
In the 1970’s the identified the phenomenon of respiratory sinus arrhythmia, which is the rise and fall of HRV as you breath. Inhaling quickens the heart rate. Exhaling decreases the heart rate. (I learned this in yoga class a long time ago.)
-
The Baroreflex is a nervous system feedback loop linking blood pressure with heart rate.
-
There are a number of different ways to measure HRV
- Time domain measures
- Frequency domain measures
- Time series analytic techniques such as Fourier Transform are used to evaluate the power of each frequency range. (We start to get over my head here, though I’ve benefited from some help doing similar analysis on my own tremor data.)
- The frequency categorization of HRV described by Dr. Ahn involves the following bands:
-
- High Frequency (~.35Hz) associated with respiratory sinus arrhythima
-
- Low Frequency (~.1 Hz)associated with baroreflex
-
- Very Low Frequency (~.025 Hz)associated with temperature regulation and certain hormonal influence, including reproductive hormones and steroids
- 4 Ultra Low Frequency associated with thermoregulation, other hormones, including cortisol, and circadian rhythms
-
- (I do not know what the difference is here between “temperature regulation” and “thermoregulation.” This could be a mistake on the slide or a real distinction I missed.)
- The low and high frequency cycles can be evaluated within a few minutes. The variable low frequency and ultra low frequency require 24 hour measurement.
- High frequency range (.15-4Hz )is associated with the parasympathetic system.
- Non-linear measures
-
Dr. Ahn then goes to the cellular level and talks about the pacemaker cells in the sinoatrial (SA) node. If you would like to follow at this level of detail, definitely watch the video. His explanation is very clear. (It begins at about minute 28:30.) The upshot, however, is that only where there is normal sinus rhythm, with heartbeats originating in the SA node, will HRV provide insight into parasympathetic activity. Therefore Dr. Ahn describes the correct beat-to-beat interval to measure as the “NN interval,” rather than the more commonly seen “RR-interval”.
- Here is a short description on stack exchange with references: What is the difference between RR-intervals and NN-intervals in HRV-data?
-
Therefore, HRV, which comes from an analysis of the time between heartbeats, has to be evaluated in the context of other data that can indicate whether there is a normal rhythm or a period of abnormal rhythm, such as pre-atrial contractions or atrial fibrillation. This data is available from an EKG.
-
But what about when measurement of HRV is done using a smartwatch? Smartwatches give us HRV from Photoplethysmography (PPG). They measure the flow of blood through your skin. You can’t directly tell, using traditional methods, whether and what kind of rhythm you have. A lot of abnormal beats will give you a high HRV reading with these systems, which does not reflect autonomic activation. (This part of the talk was very interesting to me.)
-
Sympathetic and parasympathetic influence on HRV have different dynamics, as might be expected since their effects are seen in different frequency ranges. The high frequency, parasympathetic-associated cycles have quick onset and offset, and respond immediately to breathing. The low frequency, baroreflex-associated cycles have a relatively delayed onset and then a slower recovery. (Dr. Ahn goes over these dyanmics in detail around minute 42:00.)
-
So what causes the respiratory rhythm in heart rate? It is because inhalation reduces the activity in the vagus nerve, which is the parasympathetic inhibitor of the “naturally” high heart rate.
- AMAZING DETAIL in this section: Dr. Ahn expresses surprise that the researchers who proved this conjecture were able to find volunteers for their experiment, which involved sticking a needle into the neck of the subject, near the carotid artery, and directly recording vegus nerve activity. He speculates that the investigators performed this research on themselves.
- Here is a video of one of them describing their recordings. He does not mention this detail and I have no idea if it’s true.
YouTube - Here is a link to the published paper: In vivo recordings from the human vagus nerve using ultrasound-guided microneurography
-
It turns out there is also respiratory influence on the sympathetic nervous system. (This is easier to measure since you can get your instruments into a peroneal nerve in the leg without worrying about pricking your carotid artery.) You can also pick up these systems using electrodermal skin conductance. This works because the sweat glands are activated by the sympathetic nervous system, and sweat will increase skin conductance. However, these show up in heart rate as lower frequency cycles.
-
If you can increase your HRV by breathing slowly, what happens if you breath very slowly, more slowly that about seven breaths per minute? Won’t that change the dynamics and possibly mess up the distinction between high frequency parasympathetic-associated high frequencies and the lower frequencies? The answer is yes, and some details are explained at minute 47:00.
-
The result of these interactions is what is described in Dr. Ahn’s talk as “the coherent state.”
- Interestingly for me, he uses a figure created by HeartMath. Some of the earliest talks about HRV at QS meetings discussed the Emwave device from HeartMath, and the Emwave was the first instrument I saw and used to output an HRV-based measurement. (I don’t think it gave an actual number; I seem to remember red and green lights, though I may have this mixed up) I had lost track of them until I saw this slide.
-
The coherent state, according to Dr. Ahn’s report of current research, occurs at .1Hz, or 10 seconds per breath. Dr. Ahn mentions a popular belief that this coherent state “retrains” your autonomic nervous system in a way that is beneficial to health. He finds this interesting, but he does not have research to support this idea.
-
Now that we know we are measuring “NN-interval” and why, Dr. Ahn’s talk turns to the analytical details. There are four main HRV values in use:
- Standard Deviation of NN-Interval (SDNN)
- Risk of mortality in cardiac patients
- Standard Deviation of 5-minute averages of NN-Interval (SDANN)
- Predominant circadian rhythm
- The Root Mean Square of Successive NN-Interval Differences (rMSSD)
- Vagal modulation of heart rate.
- The Percentage of NN-Intervals that Are Greater than 50ms Different than Prior NN-Interval (pNN50)
- Sensitive to uneven beat detection.
- I can imagine being interested in knowing how a device calculates HRV, but I do not do any work myself related to selected these calculations, so I didn’t bother noting more details, but Dr. Ahn begins discussing them at about minute 54:00, and even provides a glimpse of the calculations involved — probably enough to follow up on if interested.)
- Standard Deviation of NN-Interval (SDNN)
-
That’s it for now
I will probably take notes on part 2 of this lecture and post them when done. Here’s a link to the next event, September 13, if you want to view it yourself.
Heart Rate Variability: Antiquated or Indispensable? Part 2