Meeting with cardiologist, Dr. Yang. She believes, based on Zio data, that the PVCs are caused by Ventricular Ectopy. I found this basic explanation: https://www.heartlungcirc.org/article/S1443-9506(18)31918-8/fulltext
Sorry to hear of your condition and wishing you a speedy recovery.
I have a collection of thoughts on this problem.
Have you had a sleep study to confirm it is not being aggravated by sleep issues.
Does your blood work come back normal on sodium, potassium, etc.
Are catecholamine levels measurable in blood (your referenced article)
Have you reviewed all you medications and supplements for heart effects. I would google specific questions, since it doesn’t seem to show up on typical side effects lists. As an example, at one point I was on a beta blocker to slow my heart rate. It did have that effect (60 second step test went from 56 to 57 BPM). However at one point I drank a glass of cold water and my pulse went to 135 in seconds. Apparently it sensitized my heart muscles and the cold water in my esophagus chilled them and triggered that response.
Excess potassium (bananas are one source) apparently can also be a problem.
I recall a disputed approach on measuring food sensitivity using heart rate changes (15 minute window after eating).
Blood chemistry is a primary signaling path for the heart. Have you considered your microbiome?
I am also concerned your one button approach will sensitize you to the problem and that tracking it will make it worse. Did the Zio data have an accurate time stamp and give magnitude information? I am wondering if you can see the problem starting in Zio data and then when you notice it and push the button it gets worse. I wonder if taking the opposite approach of doing a relaxation routine when you notice it would reduce the severity and/or duration. Smelling essential oils, playing relaxing music with headphones (more immersive), meditating (I like and have measured the effect of Jon Kabat Zinn Full Body Scan on myself) when you notice the symptoms vs at a specific time of day.
Can you passively detect the problem with a chest strap heart rate monitor?
I have heard of people taking a modified MyZio bedside sleep monitor and using the headband on their chest to capture raw heart electrical signals via the serial port to passively collect data (I haven’t tried this).
Would the latest generation Apple Watch detect this problem and record it for you?
Take care.
A wealth of very good ideas. Your tip about cold water is very interesting. One of my favorite things to do is to swim in cold water, including in the Pacific here in the Bay Area where temps can be in the mid-fifties Fahrenheit. There is a lot of conflicting advice on sports forums about the effect of beta blockers, so I’ll proceed cautiously here.
I have a strong interest in exploring simplest factors first, looking for the easy wins. So I’m going to ignore microbiome for now. Too much noise there, I think.
Your question about whether focusing on the problem makes it better or worse is excellent, and I’ve wondered this too. I have my Zio Patch data (PDF format) now, and my main goal was to see if my one button data was roughly in agreement. But I hadn’t thought of looking to see if pressing the button typically led to more arrhythmias. Of course the existence of a button press makes subsequent presses more likely, due to the positive feedback cycle that arrhythmias initiate. This is different than the effect of noticing. But maybe I can compare PVCs that are noticed (with a button press) to PVCs that are shown by the Zio but have no button press. I think this is your suggestion, and if I can get the windows right and a simple method going I’ll do it.
My fasting blood work is normal but that doesn’t mean fluctuations in sodium and potassium aren’t having an influence. While there isn’t a way to get continuous measures of these (or even good home tests), I do think that my hydration and exercise influence the arrhythmias, and that could point to electrolyte issues. Not obvious how to explore this, but it’s on my mind.
There’s no easy way yet to test for catecholamines regularly, but since these are associated with autonomic arousal I think any exploration that tracks stress/anxiety would get me into the relevant area. I know for sure that the arrhythmias are worse when I’m on alert: a tense conversation, being about to give a talk, or being started awake by the phone can initiate the PVCs. I can also reduce the arrhythmias by doing a breathing exercise. In a way I’m less curious about this trigger since it’s so obvious.
I’m currently drinking no alcohol and eating no sweets, since both of these seem like they trigger the PVCs. But in this case I don’t really have good evidence. Like this supplements I’m taking, it’s more grasping at straws. After the next phase of evaluating my 1-Button observations compared to the Zio I may assess some of the interventions.
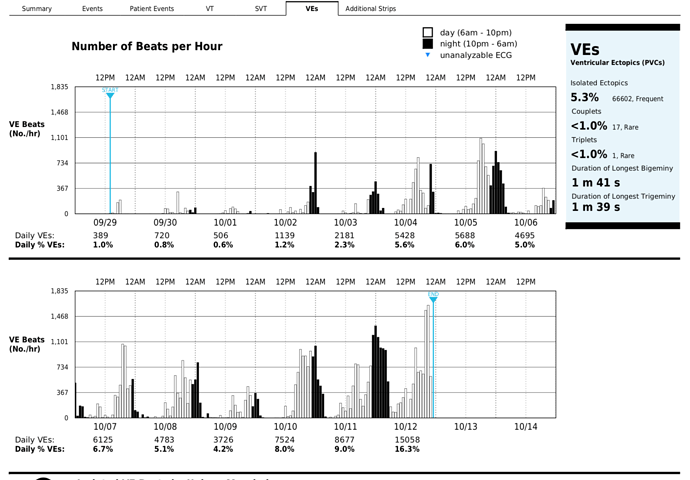
Zio Patch report uploaded here, in case anybody would like to take a look. (I would have appreciated being able to see a sample report before I started the tracking period with this system.)
Excellent meeting of the Open Humans Self-Research group this morning. I showed the Zio report alongside my 1-Button data. Some discussion points:
Obviously the 1-Button presses are fewer than the Zio-reported PVCs, because:
- Zio counts at night while I’m sleeping.
- Zio is more sensitive, counting every missed beat, while I’m more likely to notice when there are multiple missed beats.
- On bad days, I don’t try to count every missed beat since they are so frequent. Instead, I just make “a lot” of button presses.
We also discussed the physiology of arrhythmias, the role of vagus nerve in regulating heart rate, and the literature justifying the thresholds for treatment. There were some reflections on how the rigor of the threshold studies may be admirable but nonetheless leaves most of the influence of everyday influences untouched. The biomedical studies are looking at very dramatic outcome measures, such as likelihood of death, to set their thresholds. I haven’t yet entered the values into a table, but just eyeballing the two sets of data suggests that my 1-Button presses will be more frequent the Zio records bad days, as expected.
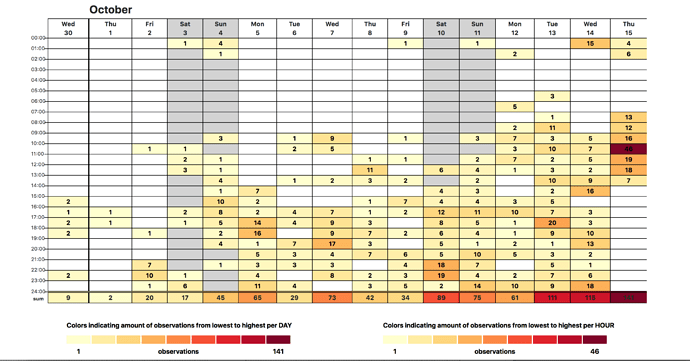
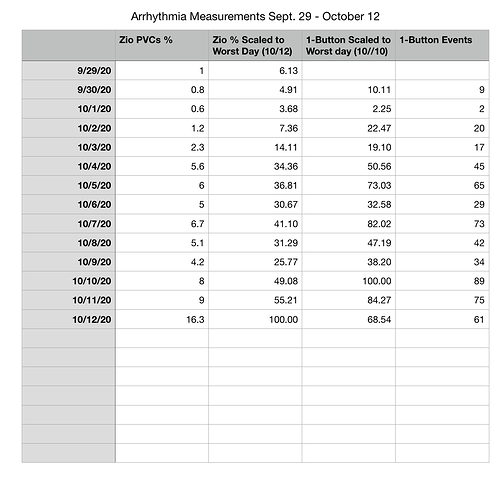
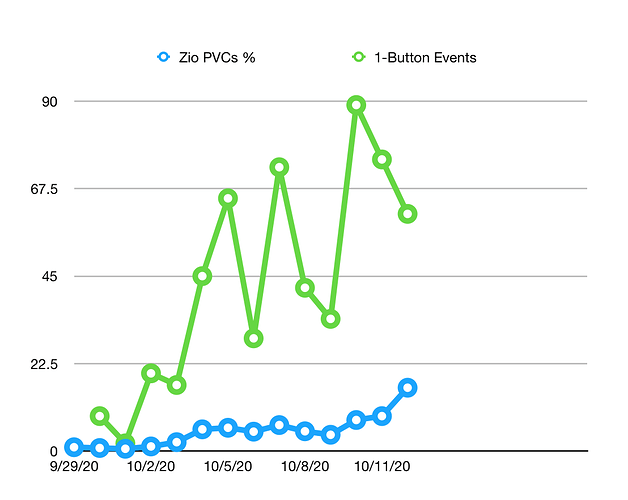
Presented my 1 Button/Zio correlation analysis research to the weekly Open Humans self-research chat. The comments and feedback were excellent. Here are some images from my slides:
Zia and 1-Button Arrhythmia Events Table:
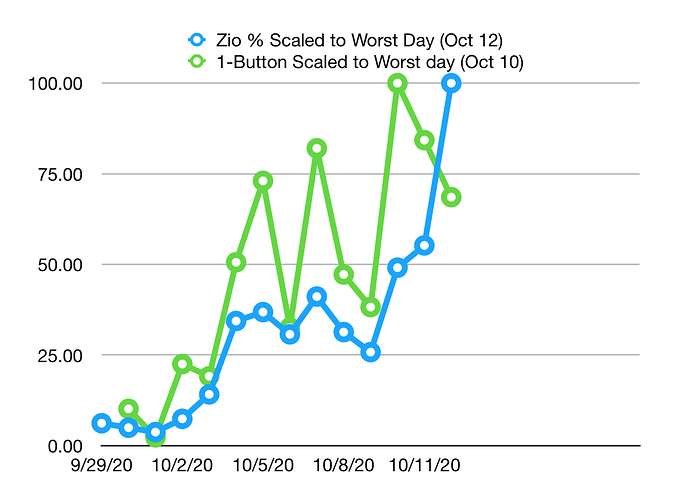
Graph of the Zio % vs 1-Button Events:
Graph of the Zeo % vs 1-Button Events Scaled to Worst Day:
The correlation is clearly worse on the days with the highest values. This may be because I stop pressing the button at the upper range of events, just lumping the whole period together as “very bad.” Also, as mentioned last week, there may be some influence of events at night: Zio reports, but I don’t press while sleeping.
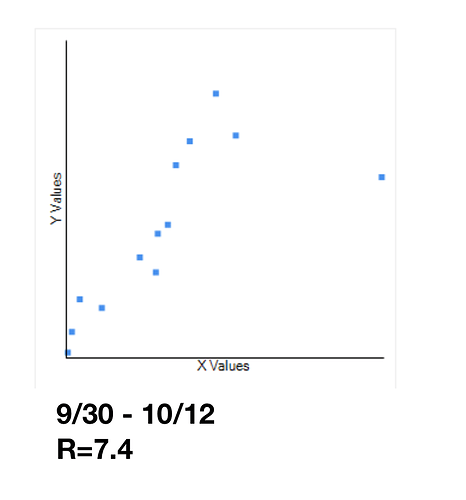
Using all the measurement days, I see a moderate correlation of 7.4:
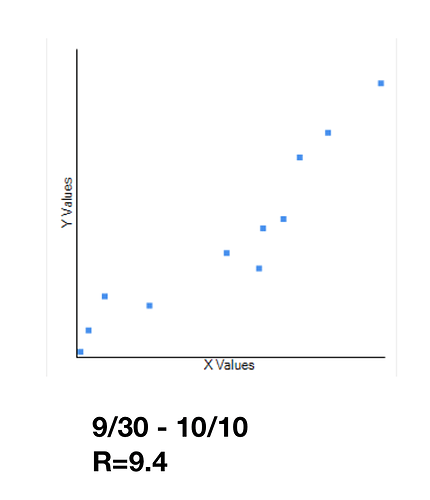
However, when I assess the correlation on the days where the Zio measurements are <50% of the worst day (10/10), the correlation is very strong: R=9.4
On a suggestion from @gedankenstuecke I may do one more additional test, setting a range of “waking hours” and checking the result. This could help tease out how much of the difference is attributable to the Zio being able to record data when I’m asleep. However, this could be a bit tricky, since I don’t go to sleep at the same time very night. And since my results are generally reassuring, it may not be worth it.
There was much discussion of interventions in the meeting. Afterwards one of the participants, Dave Blackwell, sent me this link from the blog of Dr. Anthony Pearson (aka the Skeptical Cardiologist). Pearson calls out a number of factors I believe are influencing my PVCs, including caffeine, sleep, and stress. I’m going to move on to some intervention tests in the next weeks.
With reasonable confidence in the 1-Button calibration, I’m moving to a new phase of my project. For the last 10 months, the PVCs get better and worse in waves that last a few weeks. I’ve very curious about this and have wondered what the physiological cause of a pattern of this kind. After a few days at peak shown in the chart in mid-October, the PVCs improved slowly until they were nearly gone toward the end of the second week in November. Then, last night, after a stressful event in the evening relating to family responsibilities, they sudden came back. They hit me hard until I fell asleep around midnight, and then were present strongly when I woke up this morning.
My guess is that the multi-week cycle is not a product of some kind of inherent physiological rhythm, but rather a pattern that emerges from the positive feedback effects of the PVCs themselves. The likelihood of my having PVCs in any particular hour is higher if I’ve had them in the proceeding hour. They are influenced by stress and many stress related effects have this same positive feedback pattern. (For instance, the likelihood of my having insomnia on any given night is higher if I’ve have insomnia the previous night.) Though I don’t know how to model cycles like this, and I don’t have observational data to feed such a model anyway, I think the overall pattern is obvious.
Therefore, I want to try an approach similar to my approach for dealing with insomnia. If I’m stuck in a pattern of being awake at night, I’ll take either melatonin or Valium two nights in a row. By knocking myself out the pattern, I normally do not have to take any medication on the third night, and it can be months before I’m insomniac again. This would make sense if the feedback effect is significantly driving the problem.
Dr. Yang prescribed Metroprolol (25mg) for the PVCs. She recommended I take it every morning. Onine user comments about this drug and discussions with my brother, who had it prescribed after his heart attack, made me hope to use it minimally. I’m definitely not keen on taking it every morning unless I have to.
My approach will be to take a minimal dose (12.5 mg) when PVCs increase. I’ll do this 1 or 2 times per day, every time I notice the PVCs increasing, regardless of whether they are very bothersome. My goal is to interrupt the cycle. My test period will be 3 days. This means a maximum of 75 mg over the 3 days. Then I’ll wait 48 without a dose and see if the events increase again or if they stay low. This is a five day test.
If there isn’t a strong enough effect, I’ll repeat with 25 mg per dose, with the same plan.
12.5 mg Metroprolol at 8 am.
Very soon after taking the Metoprolol I noticed the PVCs reduce. The effect was so obvious I suspected a placebo effect. The PVCs returned in the afternoon but not very strongly and I decided not to take another dose. This morning, a few PVCs, but nothing very bothersome. Also, an unusual headache this morning, wonder if this could be related to the Metoprolol the previous day.
My plan falls apart on day 1, because I thought I would continue to take the 1/2 dose of Metoprolol whenever the PVCs increased even if they weren’t bothersome, but the ones yesterday afternoon were light enough that I didn’t want to take the drug. Noticing this reluctance, I adopt a new plan. I’ll take an additional half dose whenever I’m bothered, with a limit of no more than 25 mg/24 hours.
Today, not bothersome yet.
I have been wondering about measures of stress that could correlate to your PVCs.
Galvanic skin response, although I am not sure who sells a product you could use.
Peripheral blood flow as measured by extremity temperature (Mood Ring anyone). This could be measured by using a forehead thermometer on a finger, but I expect there are many confounding factors.
Does your Heart Rate Variability show changes prior to the PVCs?
Metoprolol Side Effects does list headaches, but I didn’t find it without a direct search (symptom + drug).
Have you considered comparing CGM data with PVCs? This may detect hormonal along with diet factors.
Bothersome PVCs starting at 8:30, after a relaxed, fun meal with family. No obvious stressors. As they continued, I took a half dose of Metoprolol, 12.5 mg at 9 pm. Now 10 pm and the PVCs continue unabated. I just did a 1 minute test and there were 7 missed beats. My heart rate between the missed beats is 64 bpm. So I’m up around the 10% range during this episode. Since I took this dose after dinner, it may take more time to act. Alternately, my success yesterday could be chance, placebo, or otherwise unrelated to the drug, and this dose may in fact be too low to have an effect. I’ve decided to continue on this plan for the rest of the week and then see if there is anything obvious in the data.
12.5 mg metoprolol at 9 pm on November 11
By the time I went to sleep on Wednesday November 11 the PVCs had decreased, and then I had three excellent days. Few PVCs, no metoprolol. Today, we had a heavy lunch with wine and dessert. I drank very little (less than one glass), but that’s more than I’ve had all week. We ended the meal at 3:00pm. Unsurprisingly, I’ve been having frequent PVCs ever since, with a significant increase in the last 30 minutes. In keeping with my plan, I took a half dose of the metoprolol at 5:10.
12.5 mg metoprolol at 5:10 pm on November 15
After I took the metoprolol on Sunday the PVCs decreased within an hour:
TIME BUTTON PRESSES
5-6 pm: 15
6-7 : 2
7-8 : 1
8-9 : 1
9-10 : 0
10-11 : 4
11-12 : 9
Monday November 16 (yesterday), there was only a single press. I don’t think I’ve had such an easy day since early September.
Tuesday November 17 (today) there were no presses until late afternoon. I noticed I was hungry, tired, and then had some stress around scheduling; the PVCs started and continued for about 20 minutes. Though they weren’t too severe, they did bother me, so following my plan I took another half dose of metoprolol .
12.5 mg metoprolol at 5:45 pm on November 17.
The PVCs decreased soon after taking the metoprolol. Today they were minimal until about 3:30 pm. I had some work calls, which I made while walking around the neighborhood, and they started up near the end of the walk. I noted that they were not stress associated. I was relaxed at this time. I was a bit tired and hungry, however, and they have steadily gotten worse. Since I already ran the initial trial of “metoprolol whenever I’m bothered” longer than I expected, I’m not going to take a dose today. I’ll just eat something light right now, and see what happens.
4:10 pm: Moderately severe PVCs. No metoprolol, ate some fruit.
2:18 pm Severe PVC’s after a rare, heavy weekday lunch. 12.5 mg. metoprolol.
Multiple good days followed by a bad day yesterday. I decided not to take the Metropolol and see what happened, sitting quietly when it got too bad. This did not have much of an effect, if any. PVCs continued throughout the day and night, and then were present this morning when I woke up. At 6:50 am I took a half-dose of Metoprolol. I doubted it would work well, since the PVCs were so well established by this point. In my mental model, the beta blockers interferes with the effect of autonomic activation on heart rate. Therefore, if the PVCs are well established, even though I’m not otherwise stressed or activated, it might not work. But my expectations were not correct. Within 30 minutes my PVCs were significantly reduced. Just one or two button presses since taking the medication.
12.5 mg metoprolol at 5:50 am on November 24.
Few PVCs until 30 min. ago. Decided to catch this wave just as they were getting going.
12.5 mg metoprolol at 4 pm on November 25.
Decreased after dose, then rose again at the end of the night.Up late cooking for a holiday.
12.5 mg metoprolol at 11:55 pm on November 25
Renewed PVCs after late night and Thanksgiving meal. These doses are becoming frequent enough that I’ll stop making a separate log entry for each one, and keep them on a separate list.
12.5 mg metoprolol at 11:30 pm on November 26
This is clearly a transition phase in my project. Some things from the last 2 weeks:
-
Operational: Small details matter. I knew this already but somehow I have to relearn it with every project. I thought it was sort of dumb to enter every Metoprolol dose in the Project Log here, knowing that new forum entries generate email and new post updates to everybody who is following a topic, unless they mute them. I want to have my project be public, but I don’t want to generate excessive notifications. So I switched to tracking my medication in a separate sheet to update here more intermittently. Bad idea. Now I had two different notebooks going, and my routine was interrupted, and I lost some confidence in my notes overall. The good thing about using a project log here is that my updates are time stamped on the forum, and I have forum moderation as part of my work routine, so this helps with the cadence of the project. Lesson: Keep it simple. How many times will I outsmart myself before I just capitulate? I’m moving all my notes back here. If anybody is getting notifications who doesn’t want them, just adjust these in your forum settings.
-
Physiological: The metoprolol continues to work very well in reducing the PVCs, but I had a couple of odd symptoms that occurred for the first time last week. The first symptom was a kind of “brain buzz” like an electric shock in the back of my skull, not very painful but very odd and disturbing, followed by a slight headache and feeling of disorientation that lasted about an hour. The second was a strange reaction to cold that caused my toes to turn white and then red and swell up. This lasted in its severe form about two hours after working outside and then subsided over a couple of days. I didn’t find anything useful about the brain buzz, but I did locate some research on the feeling in my toes once my primary care NP talked it over with me and introduced me to the right search term: Raynauld’s syndrome. He described this as a rare but not unknown side effect of beta blockers. I did find some published reports of this, including a relatively recent (2016) meta-analysis: Peripheral vasoconstriction induced by β‐adrenoceptor blockers: a systematic review and a network meta‐analysis. My symptom wasn’t too bad, just worrisome, and I decided not to let it stop me from getting the benefit of the metoprolol for now.
In my reading on metoprolol and other beta blockers, it looks like there is some rebound effect associated with using the drugs. I haven’t analyzed my data yet to see if PVCs are worse in some window after a series of doses, but there’s no question that they are reduced in the 6 hours or so after I take a dose and then come back some time after. Therefore, for my next phase of the project, I’m going to change my dosing. Rather than taking 12.5 mg whenever the PVCs become severe, I’m going to take 12.5 every morning and another 12.5 dose 12 hours later. I think this will turn out to be about 6 am/6 pm, but let’s see.
For the sake of having everything in one place, here are my doses since November 28 (all 12.5 mg):
November 28 6:18 am
November 29 1.00 pm
December 2 11:55 pm
December 6 5:15 am
Finally: the bad news. I had some device issues that caught up with me yesterday, when I found that I’d lost all my data from December 6 to December 10. There had been an issue in the original firmware resulting in data loss when the device was out of power. The current 1-Button uses so little power that it doesn’t need to be charged very often, and I completely got out of the habit of charging it. AND, I never updated to the latest firmware over the summer when the data loss issue was fixed. So, on the evening of the 9th, I ran out of power, and lost my data going back to December 6, when I last connected it. I have now updated the firmware and come to terms with my loss. I did curse though.
Some additional notes:
Painful toes started December 5, mostly resolved December 6
December 6 left the device where I couldn’t get to it in the morning. Many presses unrecorded. Estimate: 30 presses between 4 am and 6 am. PVCs diminish starting around 5:45 am. Now 6:35 am and no PVCs.
December 6 12:30 pm after coaching soccer, PVCs ramping up again. I can’t remember if I took a second Metoprolol dose, my protocol says I should have but I failed to note it.
Conclusion: Since my data is missing December 6-10 and I had possibly one missing metoprolol dose during this time, and since I’m changing my protocol starting today, I’m going to mark those days as a transition time between project phases. The next phase will be: regular cadence of metoprolol dosing. My positive expectation is: My PVCs will drop to a manageable level and stay there without these regular increases in severity. I won’t have renewed symptoms that could be side effects. I’ll find it easy to manage routinely. My concerns are: I’ll have new symptoms that could be side effects, I’ll miss doses and find them hard to record regularly, I’ll develop a tolerance to the drug and have to increase my dose, I’ll have to stop the drug due to new symptoms and this will produce problems due to withdrawal.
Let’s see what happens.